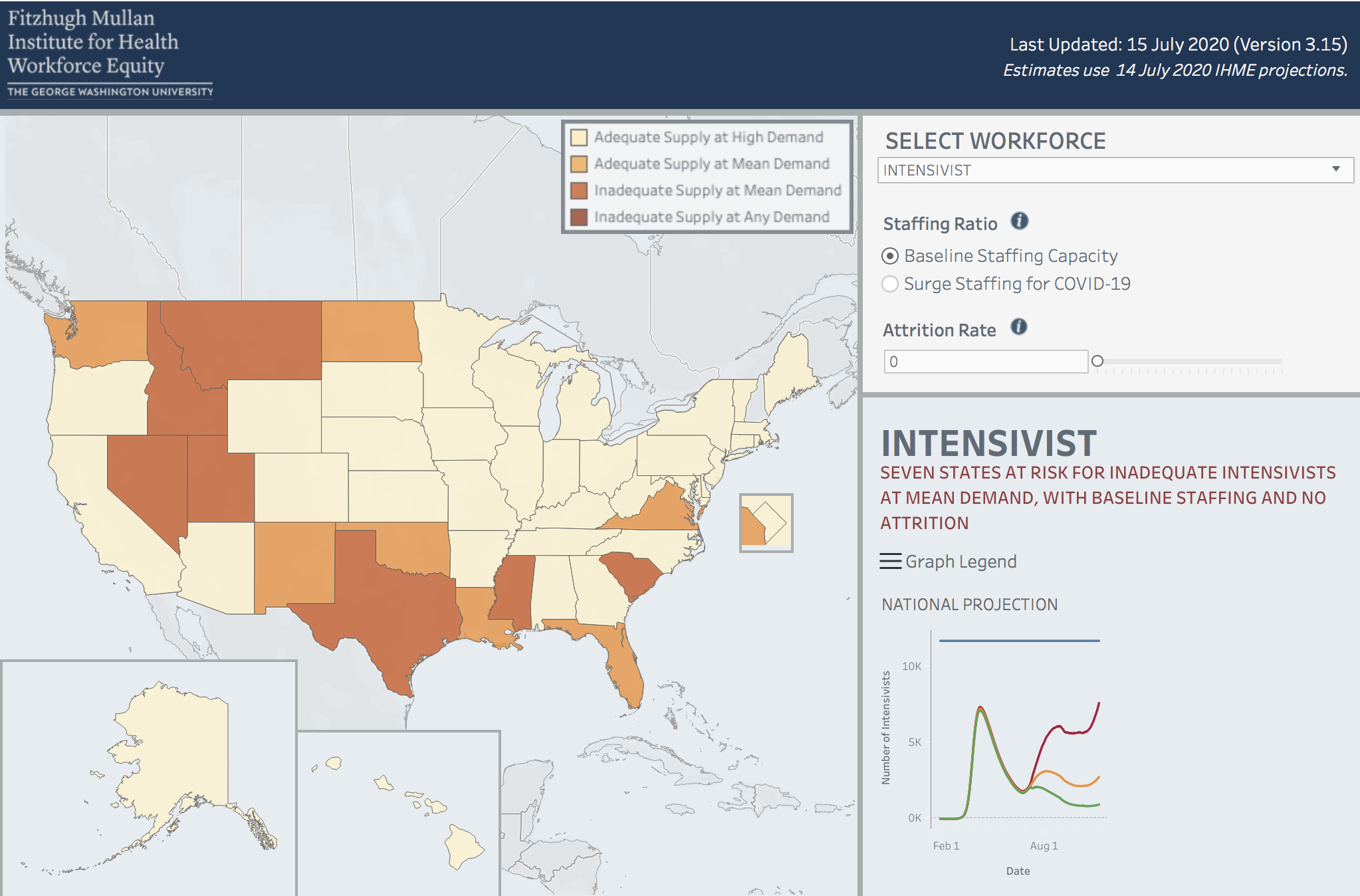
WASHINGTON, D.C. (July 23, 2020) — A hospital workforce estimator developed by the Fitzhugh Mullan Institute for Health Workforce Equity (Mullan Institute) at the George Washington University Milken Institute School of Public Health (Milken Institute SPH) shows seven states with surging COVID-19 rates are currently at risk of running out of intensivists, doctors who are trained to work in intensive care units (ICU). Seven more states have less than 50 percent of intensivists available to care for their non- COVID patients, according to a weekly update by the Mullan Institute.
“This update shows that Idaho, Mississippi, Montana, Nevada, South Carolina, Texas and Utah all could face a shortage of intensivists needed to treat these critically ill patients,” said Patricia (Polly) Pittman, PhD, director of the Mullan Institute. “Our estimator suggests that a rapid increase in severely ill COVID-19 patients could overwhelm understaffed ICUs in many states.”
While the media has largely focused on the danger of depleting ICU beds, workforce shortages to staff these units can be an even greater problem. New beds can be set up in other hospital units, or even outside the hospital setting, but ICU staffing is relatively finite. The Mullan Institute estimator allows states to anticipate shortages and provides resources on emergency measures that can be used to quickly to attract additional professionals.
Pittman and her team developed the State Health Workforce Deficit Estimator to help states and the federal government gauge the demand for health care professionals under different scenarios of infection rates and attrition – or the loss of health care workers due to illness or other reasons. The estimator allows state and federal policymakers to plan for looming spikes in COVID-19 cases and prepare by staffing up with critical workers such as ICU doctors or intensivists, critical care nurses, respiratory therapists and pharmacists.
Using data from the Institute for Health Metrics and Evaluation on the demand for service, Medicare claims data and other publicly available databases, Pittman and her colleagues looked at the availability of health care workers needed to care for the estimated number of COVID-19 patients.
In addition to the seven states facing a shortage of intensivists to treat COVID-19 patients, the team also looked at the ICU doctors needed to treat non-COVID patients during the same period.
They found that another seven states, Alabama, Arizona, Florida, Louisiana, North Dakota, Virginia and Washington would not have enough ICU doctors to treat all of the other very ill patients – people who have been in car accidents and others who need intensive medical care to survive.
The timing of the shortfalls varies by state, but Florida, for example, can expect to see this gap in ICU doctors continue to grow until early November. Texas’ surge of COVID-19 patients is expected to peak in late August.
The federal government could help by identifying states with the most serious shortfalls and deploying military health care workers to support the existing workforce.
The State Health Workforce Deficit Estimator has an interactive map that shows state-by-state shortfalls in health workers needed to meet the COVID-19 demand. A report based on the available data as of mid-July can be accessed here.